SYDNEY, N.S. — Nova Scotia Health says there are several reasons for the higher than expected death ratio from the Cape Breton Healthcare Complex in 2019-20 and that work has already begun to improve those numbers.
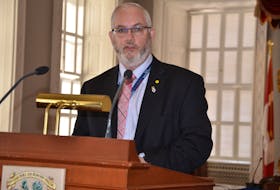
In fact, the most recent numbers from April to September 2020 are already indicating an improvement with a Hospital Standardized Mortality Ratio (HSMR) of 119, says Dr. Ward Patrick, senior medical director for critical care for Nova Scotia Health.
“I do believe that last year’s data, the 143, is not something that we can ignore,” said Patrick during a Zoom call from Halifax. “But I’m hopeful looking at the data we’re seeing here today now that it was an aberrant year and that we are actually on track to meet the national average for the first time. Even if we meet the national average, that’s not where we stop. We want to actually be the best in the country in terms of HSMRs.”

Data for 2019-20 from the Canadian Institute for Health Information (CIHI) had indicated hospitals within the Cape Breton Healthcare Complex have been recording death rates much higher than the national average. In 2019-20, the Cape Breton Healthcare Complex recorded an HSMR or death rate ratio of 143. That’s compared to the national average of 95 for Canada over the same time period. In the past five years, the complex has consistently been above the national average with 124 in 2015-16, 133 in 2016-17, 158 in 2017-18 and 133 in 2018-19. Those numbers are supposed to exclude stillborns, those discharged against medical advice and palliative care patients.
For the four hospitals of the Cape Breton Healthcare Complex (Cape Breton Regional Hospital, Glace Bay Hospital, New Waterford Consolidated and the Northside General), there are 4,139 HSMR cases with 421 total observed deaths and 293.61 total expected deaths for a difference between observed and expected deaths of 127.29, according to Nova Scotia Health.
Just the fact that there are four hospitals contributing to the results from the Cape Breton Healthcare Complex has affected the numbers, says Patrick. For example, when other hospitals report their lengths of stays, they only record the number of days each individual patient remains in that particular hospital whereas within the complex hospitals, a patient could transfer from New Waterford to the Cape Breton Regional, creating a longer total length of stay which impacts negatively on the final results. The four hospitals included within the complex make up the required numbers to be included in the CIHI study.
Another reason for the higher than expected numbers is the continued presence of palliative care patients not being properly coded which has negatively impacted the complex’s score. As well, when a patient is discharged, their medical record (chart) is coded by Health Information Services. It is this coded information that is submitted to CIHI. If this chart doesn’t include a proper discharge summary, that too can impact coding accuracy. To improve accuracy, Nova Scotia Health has undertaken several measures such as placing a patient alert flag for palliative care patients, that charts are reviewed by two different coding staff and having all coding and abstracting staff complete refresher training on palliative care coding standards.
An antimicrobial stewardship program has also begun for all zones which will develop guidelines for broad-spectrum antibiotics and management of common infectious syndromes, as well as guidelines for sepsis, pneumonia and urinary tract infections. A sepsis care directive has been developed for use in emergency departments and a review has started for the early warning signs of deteriorating patients in the central and eastern zones.
Patrick says the new numbers in December came as a shock since Nova Scotia Health had undertaken measures to improve the statistics and those measures appeared to be working everywhere else but Cape Breton.
“So the question is, what’s different there and the way we’re going to answer that is to actually look at the charts at the Cape Breton Healthcare Complex and see if there is anything different,” says Patrick. “And that plan is actually underway now.”
A group of doctors locally will be examining why the Cape Breton Healthcare Complex keeps having higher HSMRs. The group will also examine problem areas with the largest gaps between expected and observed deaths such as chronic obstructive pulmonary disease (COPD), heart failure and sepsis, to see where further changes are needed.
“We know that we have to look at this and make improvements,” Patrick adds.
Elizabeth Patterson is the health reporter at the Cape Breton Post.